Case Study
Estimating the
obesity-attributable
risk of cardiovascular
disease (CVD)
The Question
Obesity rates in the United States (US) have grown rapidly over the last 20 years, with current prevalence estimated at ˃40%. Obesity is a known risk factor for CVD, and GLP-1-based therapies for weight loss have been shown to reduce the risk of major heart events as well.
The mechanisms through which this reduction occurs and the potential impact of these drugs on population-level CVD burden in the US, however, are not well understood. Current estimates are limited by a focus on the direct effect of obesity on CVD, use of non-representative data sources, and a reliance on inaccurate diagnosis codes.
The Approach
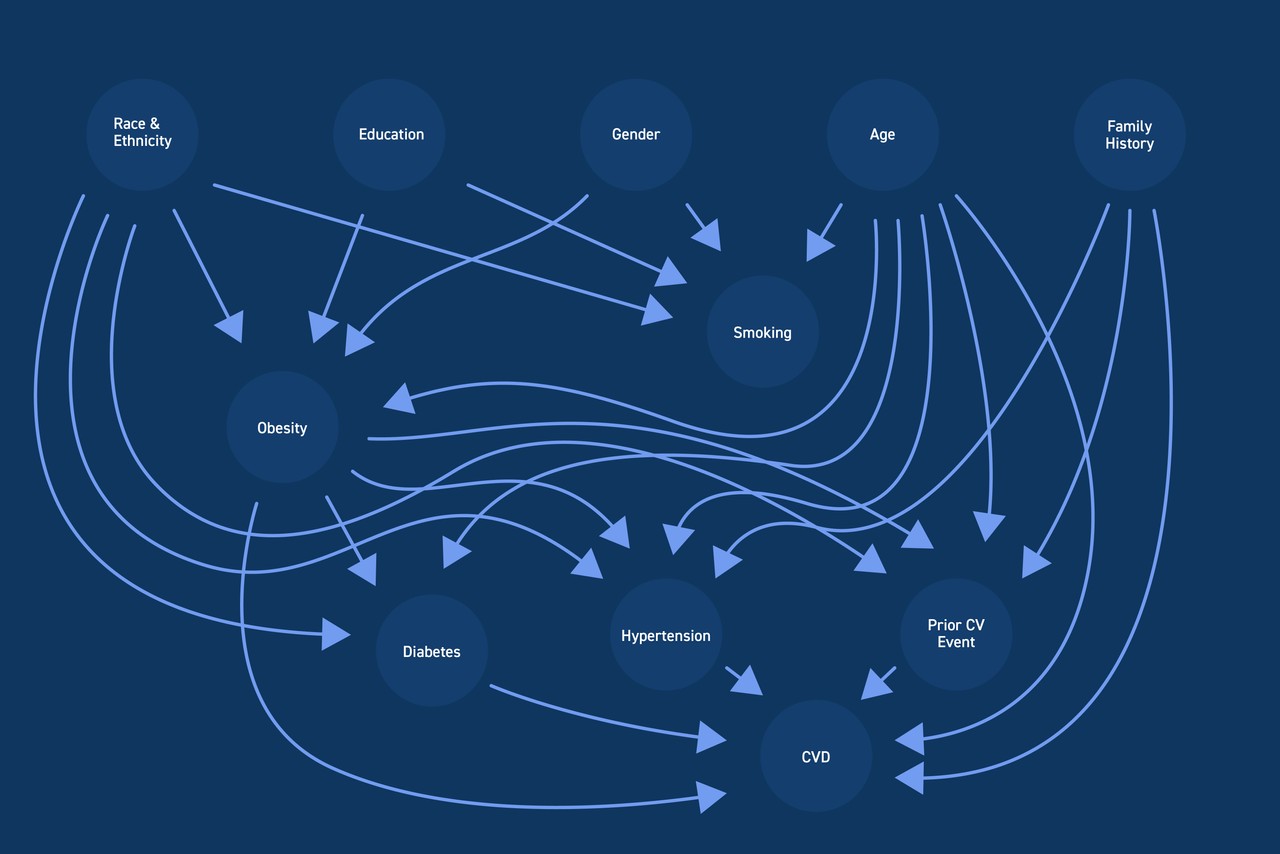
Nationally-representative, cross-sectional NHANES data were adapted to produce longitudinal estimates of weight by shifting the time axis from wave years to participant age. To fully map out the constellation of CVD risk factors, a Bayesian network (BN) was developed. The BN structure was learned through a combination of expert knowledge and constraint-based optimization, with conditional probability distributions encoded in each network dependency via logistic regression. Counterfactual predictions from the fitted BN were generated to estimate the population attributable fraction (PAF) of CVD due to obesity, and the direct and indirect pathways through which changes in CVD risk occur were characterized.
CVD cases from 2024-2035 were estimated using prevalence projections from a weighted logistic regression model fitted to 2009-2020 NHANES data and Census population projections. The BN PAF was then applied to projected CVD cases to estimate the number of CVD cases attributable to obesity in the US from 2024-2035.
The Results
The final sample included data from approximately 29,000 participants. PAF estimates from the fitted BN indicated that 19% of CVD cases were attributable to obesity, with approximately 80% of this burden due to the indirect effect of obesity occurring through intermediate risk factors (hypertension, type II diabetes, and prior cardiovascular events).
Of these risk factors, reduced hypertension played the largest role, accounting for 48% of the effect of obesity elimination on CVD. Type II diabetes and prior cardiovascular events each represented approximately 15% of the indirect effect of obesity on CVD. Based on BN PAF and CVD projections for 2024-2035, eliminating obesity was estimated to avert over 6 million CVD cases in the general population during this time period.
The Long And
Short Of it
Through an innovative adaptation of NHANES data combined with a sophisticated network modeling approach, we generated population-level estimates of current and projected CVD burden attributable to obesity. Results highlight the full impact of obesity elimination, provide insight into the nature of this impact, and can be used to support payer discussions regarding coverage of novel weight loss therapies.