Case Study
Understanding patient
outcomes in co-pay
accumulator adjustment
programs
The Question
Copay accumulator adjustment programs (CAAP), implemented by pharmacy benefit managers, distinguish between medication copay costs borne by patients and those subsidized by manufacturer copay assistance.
For patients, subsidized copay assistance does not count towards patient deductibles. As a result, patients with high-cost therapies may face a higher out-of-pocket burden before their deductible is met. These programs are expanding in response to employer concerns about rising healthcare costs, even though their impact on patient outcomes remains unknown. Our client wanted to know: are these programs making it harder for patients to start and stay on specialty medications?
The Approach
We used pharmacy claims from large, self-insured employers before and after they implemented a copay accumulator adjustment program.
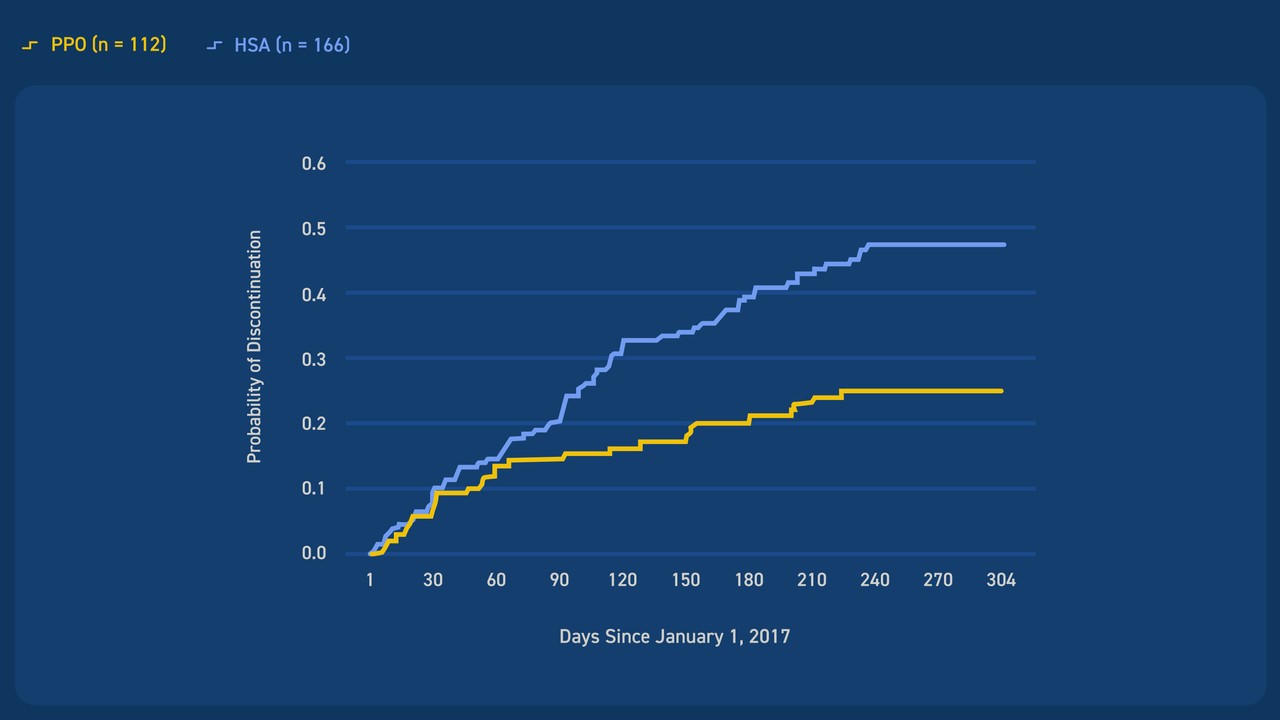
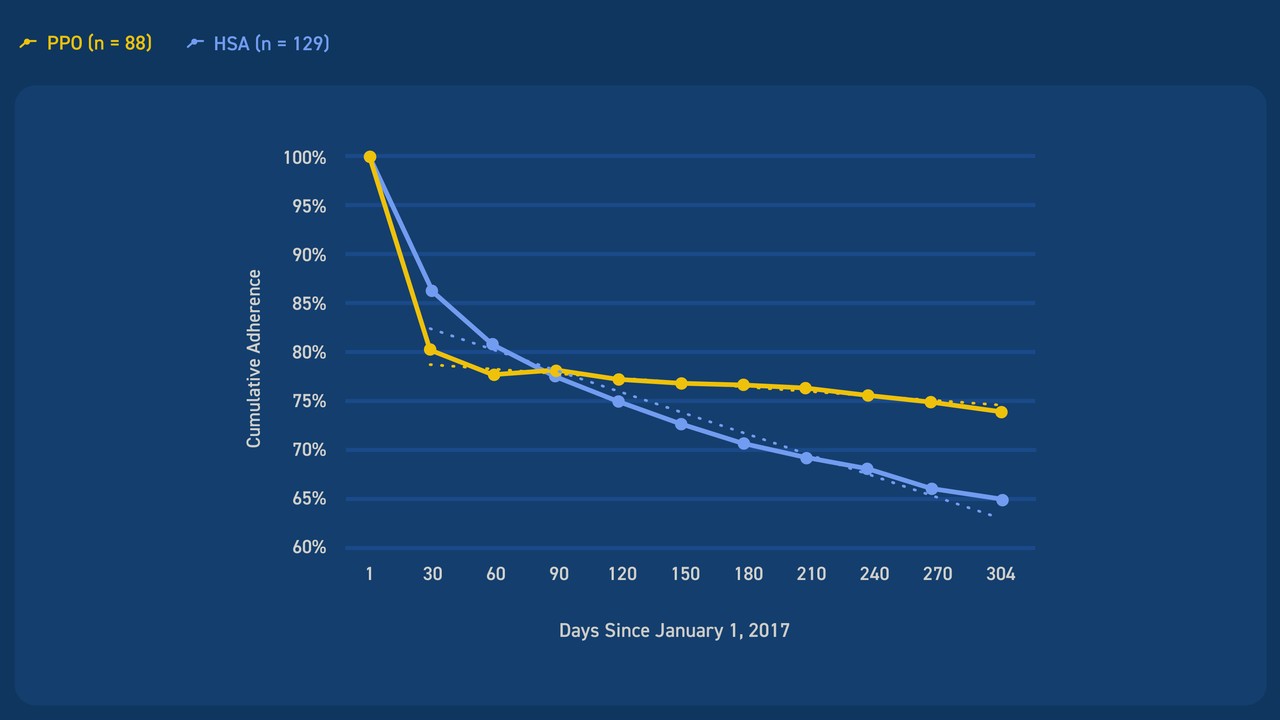
We identified patients treated with autoimmune specialty drugs and compared treatment patterns over time. We separately evaluated patients with health savings accounts and those with preferred provider organization plans, as patients with health savings accounts were expected to face higher deductibles.
The Results
Patients with health saving accounts had lower adherence and higher discontinuation of specialty drugs following the implementation of the copay accumulator adjustment program.
The Long And
Short Of it
Our client wanted to understand the real-world impact of copay accumulator adjustment programs on patients who need specialty autoimmune therapy.
We identified a data source that allowed us to meaningfully evaluate this impact. Our findings suggest that these programs reduce specialty drug use for patients with chronic disease.