Case Study
Developing a policy
model to estimate
the impact of
a new treatment for major depressive disorder (MDD) on wider availability of psychiatry resources
The Question
Standard cost-effectiveness models are limited in that they concentrate solely on the index patient and ignore the wider context of how using often intrinsically scarce resources affects the broader health system.
Our client asked us to demonstrate the value of a therapy based on its potential to lead to less resource-intensive patient management from psychiatrists, leading to the freeing up of a key resource. It is estimated that the US has less than half of the qualified psychiatry practitioners than it needs to treat all of its patients diagnosed with mental health disorders.
The Approach
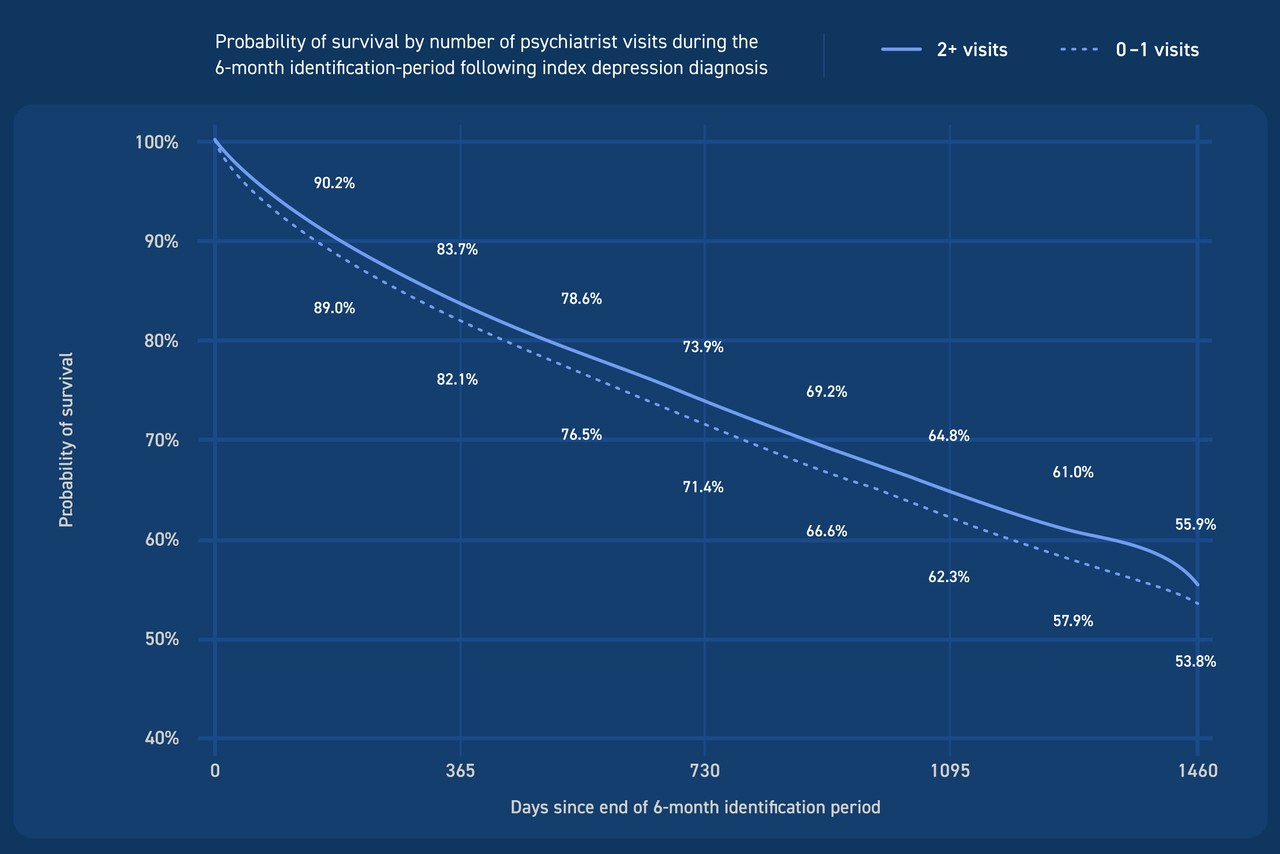
We undertook a series of analyses on real-world data sources to estimate a) the proportion of patients who would benefit from psychiatry access, b) the relative difference in downstream outcomes (costs and mortality) between those who get greater than one psychiatry appointments in the period of study and those who do not, and c) the reduction in psychiatry time needed to manage the average MDD patient when treated with our client’s therapy as compared to the standard of care.
The Results
Estimating the role of patient access to psychiatry on outcomes
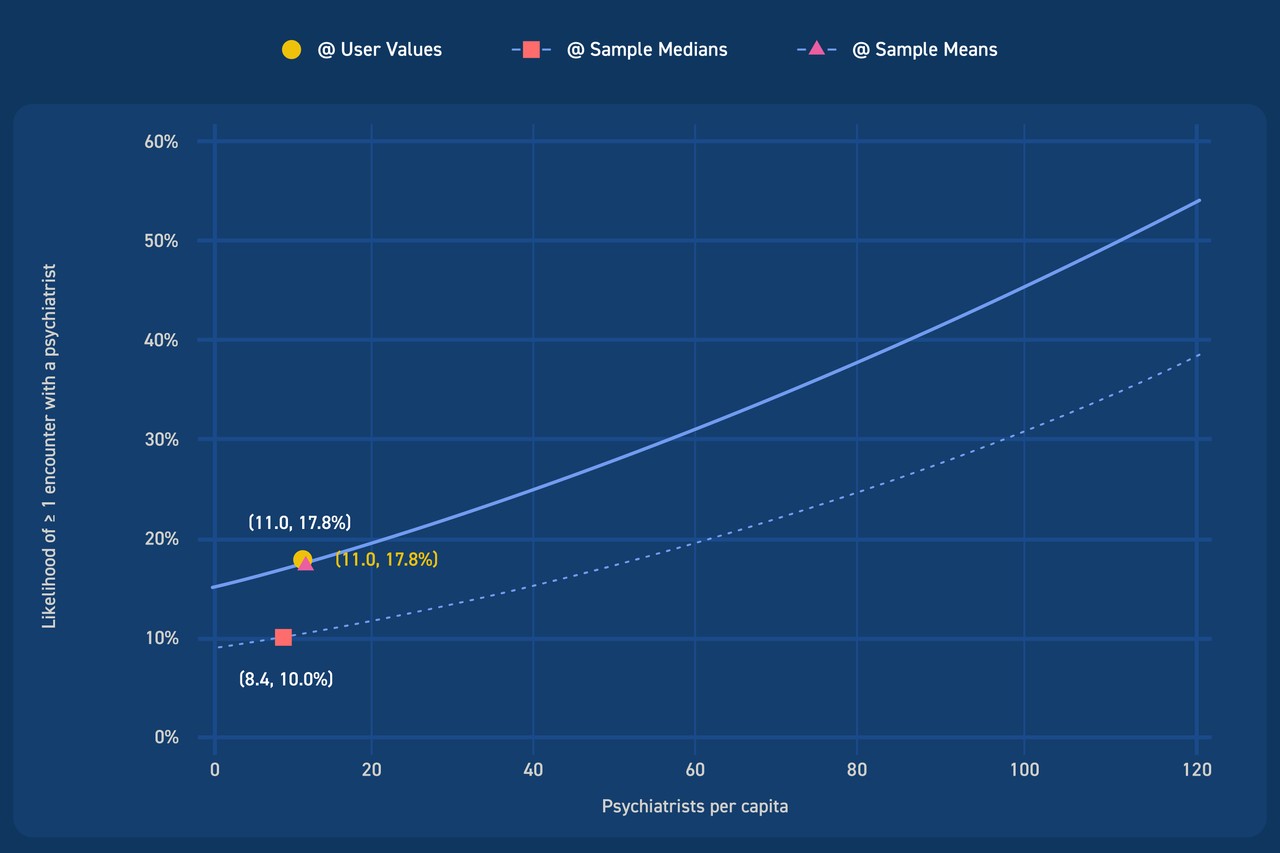
We showed that the likelihood of getting access to psychiatry care was a function of the population density of available psychiatrists in your county,
Modeling the impact of a pharmacological treatment that requires less psychiatrist time per year
Data on the estimated mean number of visits to a psychiatrist (or associated mental health professional) for patients on different treatment regimens for major depressive disorder (both pharmacological and psychotherapy) allowed us to estimate the marginal value of freeing up more psychiatry time for non-MDD patients.
The Long And
Short Of it
We helped a client with a treatment that had no marginal comparative advantage in the standard measure of efficacy (response/remission rate) over the standard of care make a strong value statement outside of the standard cost-effectiveness framework.
This also tapped into a policy dilemma dominating conversations in the mental health field: the shortage of qualified psychiatrists and psychologists to support patients diagnosed with mental health disorders.